Eligibility and benefits
Before our members’ appointments with you, ask to see their electronic or physical member ID card for current information and a photo ID to guard against medical identity theft. You should also verify their eligibility and benefits for each visit.
How to verify
Online:
Sign in to Availity® Essentials. You can verify eligibility, benefits and current primary care provider and view member ID cards. If you don’t yet have an Availity Essentials account, register here at no cost to you.
Call:
You also may call Provider Customer Service at 1-800-230-6138, Monday – Friday, 7 a.m. – 8 p.m. CT.
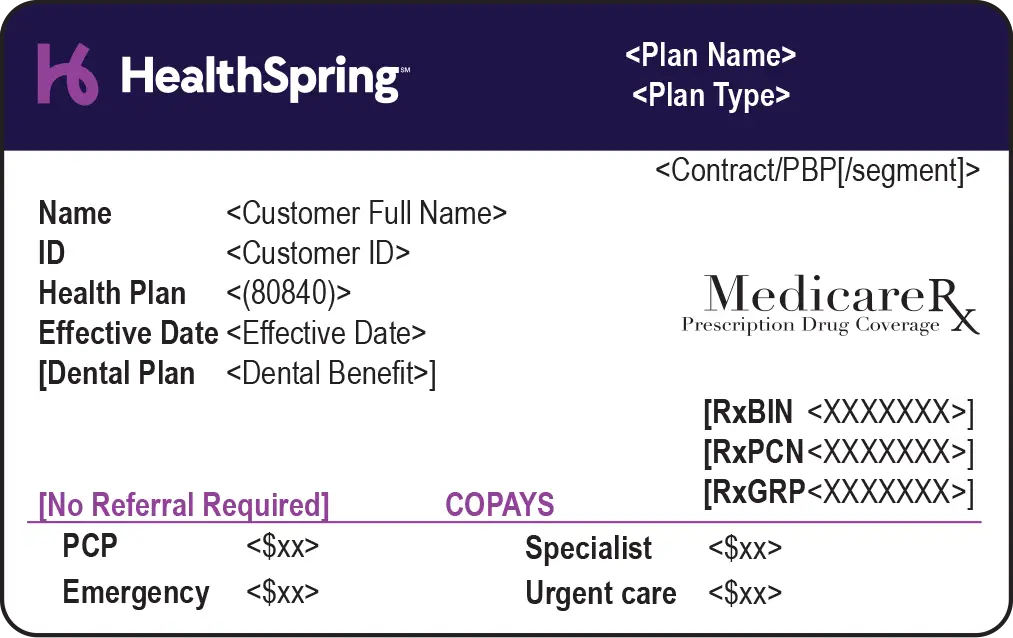
Review member ID cards
Member ID cards have helpful information, including:
ID number to use for all claims and inquiries
Effective date of coverage
Copayment due at the time of service
Dental coverage
Prescription drug coverage
Customer service numbers
You can download and save our key to member ID cards.
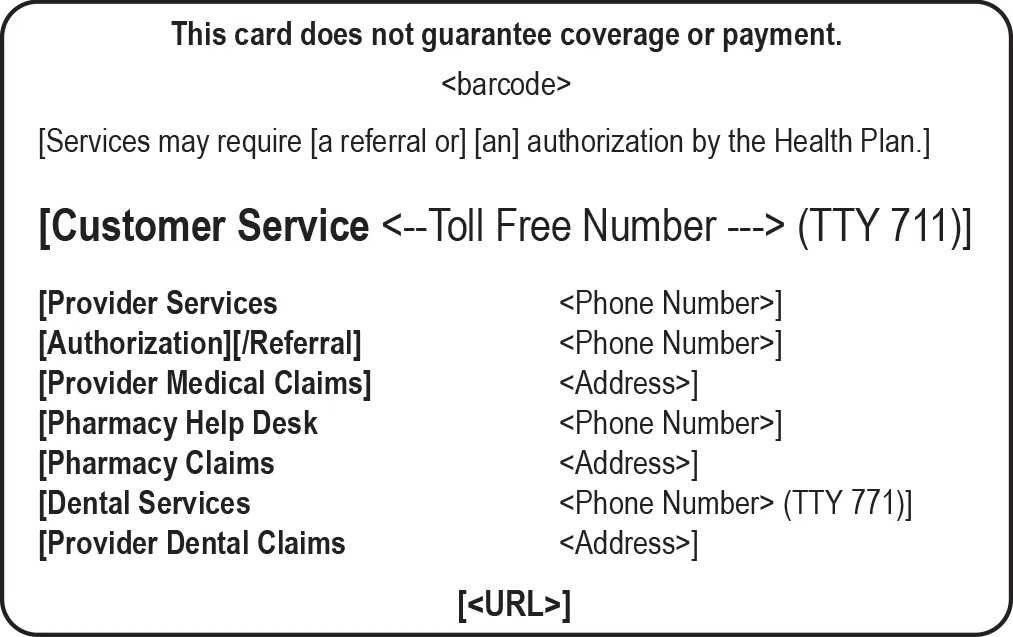
Verification of eligibility and benefit information is not a guarantee of payment. Benefits will be determined once a claim is received and will be based upon, among other things, the member’s eligibility, any claims received during the interim period and the terms of the member’s evidence of coverage applicable on the date services were rendered.
While HealthSpring will have the most up-to-date information available, member data is subject to change. The Centers for Medicare & Medicaid Services can retroactively terminate members for various reasons that can retroactively affect their eligibility. If HealthSpring pays a claim that is then retroactively terminated, our claim recovery unit will request a refund from the provider or offset the overpayment. The provider must then contact CMS Eligibility to determine the member’s actual benefit coverage for the date of service in question.