Elegibilidad y beneficios
Antes de tus citas con nuestros miembros, solicita ver sus tarjetas ID de miembro electrónicas o físicas para ver información actualizada, y una identificación con fotografía como protección contra el robo de identidad médica. También deberías verificar su elegibilidad y beneficios para cada visita.
Cómo realizar la verificación
En línea:
Regístrate para Availity® Essentials. Puedes verificar la elegibilidad, los beneficios y los proveedores de cuidado primario actuales, así como ver las tarjetas ID del miembro. Si todavía no tienes una cuenta de Availity Essentials, regístrate aquí sin costo para ti.
Llama a:
También puedes llamar a Servicio al cliente para proveedores al 1-800-230-6138, de lunes a viernes, de 7 am a 8 pm, hora del centro.
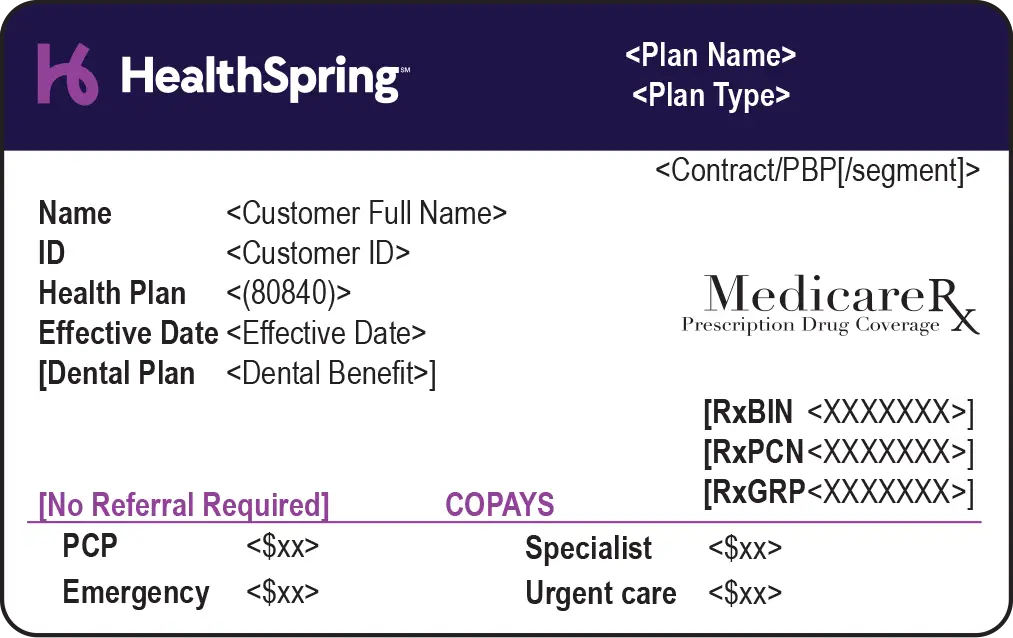
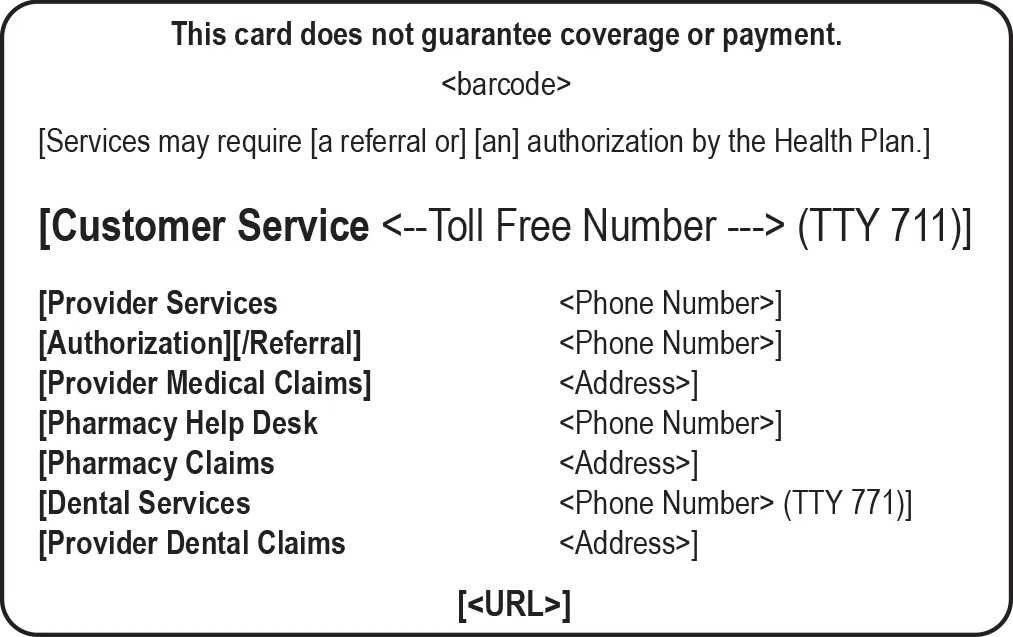
Revisar las tarjetas ID de miembro
Las tarjetas ID de miembro tienen información útil, que incluye:
Número de ID que se usa para todos los reclamos y consultas
Fecha de inicio de la cobertura
Copago que se paga al momento del servicio
Cobertura dental
Cobertura de medicamentos con receta
Números de servicio al cliente
Puedes descargar y guardar nuestra clave para las tarjetas ID del miembro.
La verificación de la información sobre elegibilidad y beneficios no garantiza el pago. Los beneficios se determinarán una vez que el reclamo haya sido recibido y se basarán, entre otras cosas, en la elegibilidad del miembro, en cualquier reclamo recibido durante el período de transición y en los términos de la evidencia de cobertura del miembro aplicables en la fecha en que se prestaron los servicios.
Si bien HealthSpring tendrá disponible la información más actualizada, los datos del miembro están sujetos a cambios. Los Centros de Servicios de Medicare y Medicaid pueden dar de baja retroactivamente a los miembros por distintos motivos que pueden afectar retroactivamente su elegibilidad. Si HealthSpring paga un reclamo que luego se cancela retroactivamente, nuestra unidad de recuperación de reclamos solicitará un reembolso del proveedor o una compensación del sobrepago. El proveedor debe luego comunicarse con el área de Elegibilidad de los CMS para determinar la cobertura de beneficios real del miembro en la fecha del servicio en cuestión.